Driving Toward a Consistent, Transparent, and Equitable Prior Authorization Process for Medicaid Beneficiaries
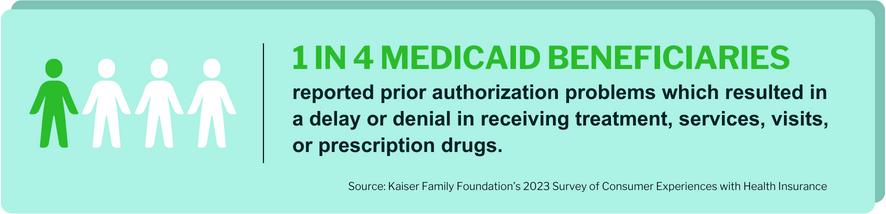
Prior authorization denial rates are in the spotlight for Medicaid beneficiaries. According to Kaiser Family Foundation’s 2023 Survey of Consumer Experiences with Health Insurance, almost 1 in 4 Medicaid beneficiaries reported prior authorization problems which resulted in a delay or denial in receiving treatment, services, visits, or prescription drugs. In the past few years, increased reports of Medicaid beneficiaries having care denied or delayed by their Managed Care Organizations (MCOs) have caught the attention of the federal government due to the potential impact on access to appropriate care.
For this reason, the federal government is making an effort to understand the current Medicaid MCO prior authorization practices at both a macro and micro level. This includes the analysis of MCO practices and a further examination of the beneficiary experience. It is through this understanding of the current prior authorization process that opportunities for future changes can be identified and implemented.

The Latest Updates with the Prior Authorization Process
To date, it is difficult to understand how the prior authorization process is working due to limited required reporting for PAs, appeals, and fair hearings for Medicaid MCOs. As of December 2022, CMS requires states as part of the Managed Care Program Annual Report to provide limited data elements on appeals, grievances, and state fair hearings data, which include the number of appeals resolved at the plan level, state fair hearing requests, and external Medicaid reviews by decision type (42 CFR § 438.66(e),).
Additional metrics were proposed by CMS in December of 2022; however, these still remain in draft. The proposed metric changes include the percentage of initial prior authorization requests that are approved and denied (CMS 0057-P – Advancing Interoperability and Improving Prior Authorization Process). Further, in spring of 2023, CMS issued two more Notices of Proposed Rulemaking (NPRMs) around Managed Care Access that will require additional reporting metrics from MCOs related to access.
Federal Government Attention on the Prior Authorization Process and Denials: OIG and MACPAC Work
In July of 2023, the Health and Human and Services (HHS) Department Office of Inspector General (OIG) issued a report titled High Rates of Prior Authorization Denials by Some Plans and Limited State Oversight Raise Concerns About Access to Care in Medicaid Managed Care. A growing number of Medicaid beneficiary complaints identified in the report were the catalyst for this congressional request to be made to the OIG. The request had the OIG evaluate whether MCOs are providing medically necessary health care services to their beneficiaries. The report summarized the OIG’s findings from analyzing 115 MCOs across 37 states, which included surveying State Medicaid agency officials on oversight of the prior authorization process. The OIG identified three main areas of concerns:
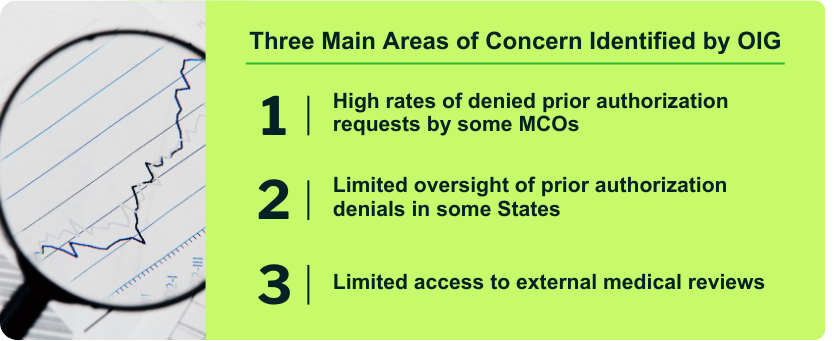
The findings from the OIG report included an average MCO PA denial rate of 12.5% for Medicaid, which ranged from the lowest rate of 2% to the highest rate of 41% across the surveyed MCOs. In contrast, Medicare Advantage plans, which have more robust federally mandated oversight process requirements, had an average denial rate of 6% in 2021 per an analysis of CMS data conducted by the Kaiser Family Foundation.
For calendar year 2023, the Medicaid and CHIP Payment and Access Commission (MACPAC) is focused on understanding the current state of prior authorization denials. MACPAC has set out to provide insights and recommendations around these key questions:
- To what extent are Medicaid beneficiaries in managed care experiencing denials and filing appeals?
- How do states and CMS monitor and oversee denials and appeals in managed care?
- Do beneficiaries find the appeals process to be accessible?
MACPAC found data on the Medicaid prior authorization process to be limited. The only federal requirement for data reporting is when beneficiaries are filing appeals. Individual states may have requirements in place for additional data collection on the PA process. MACPAC’s research is scheduled for completion in January 2024 and will include recommendations to be shared with Congress.
The initial recommendations in the July 2023 OIG report and the insights from MACPAC’s quarterly project updates detail a lack of a consistent, transparent, and equitable prior authorization process for all Medicaid beneficiaries to ensure access to appropriate care. Some states are already taking steps to ensure access to care is not limited by the PA process. While there may be challenges due to the unique nature of each State’s Medicaid programs, there are opportunities for updating processes to increase consistency, transparency, and fairness.
Opportunity to Standardize the Appeals Process with an Independent Partner
One way to address inconsistency within prior authorizations across all Medicaid beneficiaries is to have one statewide appeals process that is administered by an independent third-party. A third-party partner, like Acentra Health, is conflict free and has no financial interest in the outcome of the process. Acentra Health is not a payer and not the state. A conflict-free partner relies on a defined benefits structure, state rules, and clinical guidelines for decision making.
Acentra Health has been working with TennCare, the Tennessee State Medicaid Agency, since 2007. Acentra Health writes medical necessity reviews and testifies in fair hearings in support of denials in our role as independent medical reviewer, a critical part of the appeals process. Since 2007, we have written more than 56,000 medical necessity reviews and testified in over 45,000 hearings. Acentra Health was also a collaborative partner as TennCare worked to have portions of the Grier consent decree vacated. MCOs are responsible for the first- and second-level reconsiderations of denied services. If denied on reconsideration, the beneficiary has the option of appealing the denial to TennCare using a standard process. Through the years, Acentra Health has been able to provide TennCare data on appeal trends, which allows the state to enhance criteria and address inconsistencies with MCOs and providers. To note from the OIG 2023 report, the Tennessee MCOs have low denial rates. This includes United Healthcare Community Plan of TN and Anthem’s Amerigroup Tennessee, Inc, which have denial rates of 8.8% and 7%, respectively. Denial rates could potentially be lower due to the presence of a standardized independent appeal process which beneficiaries can use if they do not agree with an MCO’s decision.
Opportunity to Enhance Oversight of the Prior Authorization Process
Another option states have is to strengthen the quality oversight of MCO administration of the prior authorization process. Many External Quality Review Organization (EQRO) reviews site issues with the PA process, which may be followed up with more detailed reporting. Frequent consolidation and reviews of prior authorization data including denial rates, analyzing trends, and public reporting, would provide better transparency around the current state of the process. Ongoing data monitoring will allow states to identify trends in denial rates and respond in a timely manner as appropriate.
Beyond data analysis, additional oversight may include routine review of denials by a third-party independent review organization to provide an unbiased opinion on denial decisions. External reviews could be performed on a routine basis and include a random sampling or targeted selection based on identified trends. Acentra Health provides software as a service that can automatically receive, validate, and visualize data and reporting submitted by MCOs to the state Medicaid program. This type of oversight reporting can also be augmented by independent clinical reviews on specific cases by Acentra Health’s experienced team.
Utilizing Resources to Improve Medicaid Prior Authorization Oversight
As 2023 nears a close and MACPAC finishes its analysis of the current state of PA denials, additional federal guidance may be on the horizon for Medicaid PA oversight. With or without federal guidance, individual states have the opportunity to enhance their processes to ensure access to appropriate care. Experienced state partners can play a key role in helping states design and implement programs to meet their unique needs as well as being an independent, conflict-free review partner.
Acentra Health has over three decades of experience with the prior authorization process and is currently a partner to 23 states providing both services and technology for physical, behavioral, dental, emergency transport, and pharmacy prior authorizations. Our prior authorization experience includes processing PAs, appeals, and assisting states with the fair hearing process. Our appeals experience also spans Medicare as the Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO) for 29 states. To connect with our experts, visit our page here.
Other Posts You Might Be Interested In
Battling Burnout: Addressing Mental Health Challenges Among Public Sector Employees
Learn how burnout impacts public sector employees and explore statistics, causes, and solutions to help address mental health challenges.
Read MoreNational Association of Medicaid Directors 2023 Session Highlights
Discover key insights on Medicaid and other important session topics from the National Association of Medicaid Directors 2023 Conference.
Read MorePlan Ahead: Preparing for Medicaid Prior Authorization Changes
Changes are coming to the Medicaid Prior Authorizations. Find out how Acentra Health is preparing clients for the new proposed CMS rule.
Read More


